Non-Invasive Mechanical Ventilation Versus Continuous Positive ...
Maybe your like
- Home
- All contents
- Ahead of print
- Latest issue
- All issues
- Supplements
- Covers gallery
- Podcasts
- Related journal - Open Respiratory Archives
- Subscribe to our newsletter
- Publish your article
- Guide for authors
- Submit an article
- Ethics in publishing
- Open Access Option
- Language Editing services
- About the journal
- Aims and scope
- Editorial Board
- Contact
- Advertising
- Metrics
- Most often read
- Most cited
- Most popular
- All metrics
- Metrics by country
 ISSN: 0300-2896
ISSN: 0300-2896 Archivos de Bronconeumologia is an international journal that publishes original studies whose content is based upon results of research initiatives dealing with several aspects of respiratory medicine including epidemiology, respiratory physiology, pathophysiology of respiratory diseases, clinical management, thoracic surgery, pediatric lung diseases, respiratory critical care, respiratory allergy and translational research. Other types of articles such as editorials, reviews, and different types of letters are also published in the journal. Additionally, the journal expresses the voice of the following scientific societies: the Spanish Respiratory Society of Pneumology and Thoracic Surgery (SEPAR; https://www.separ.es/), the Latin American Thoracic Society (ALAT; https://alatorax.org/), and the Iberian American Association of Thoracic Surgery (AIACT; http://www.aiatorax.com/). It is a monthly journal in which all manuscripts are sent to peer-review and handled by the editor or an associate editor from the team and the final decision is made on the basis of the comments from the expert reviewers and the editors. The journal is published solely in English. All the published data is composed of novel manuscripts not previously published in any other journal and not being in consideration for publication in any other journal.. The journal is indexed at Science Citation Index Expanded, Medline/Pubmed, Embase and SCOPUS. Access to any published article is possible through the journal's web page as well as from Pubmed, ScienceDirect, and other international databases. Furthermore, the journal is also present in X, Facebook and Linkedin. Manuscripts can be submitted electronically using the following web site: https://www.editorialmanager.com/ARBR/.
See more Indexed in:Medline, Science Citation Index Expanded (SCIE)
See more Follow us: Twitter Facebook RSS Alerta email Impact factorThe Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years. © Clarivate Analytics, Journal Citation Reports 2025
See more Impact factor 2024 9.2 CitescoreCiteScore measures average citations received per document published.
See more Citescore 2024 3.5 SJRSRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See more SJR 2024 0.466 SNIPSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more SNIP 2024 0.505 Time to first decisionThe median number of days it takes for an article to go from submission to first editorial decision.
See more Time to first decision 5 days View more metrics Open Access Option Hide Journal Information Previous article | Next article Vol. 53. Issue 10.Pages 561-567 (October 2017) Export reference Share Share Twitter Facebook Bluesky Linkedin whatsapp E-mail Print Download PDF More article options Statistics Outline- Abstract
- Keywords
- Resumen
- Palabras clave
- Introduction
- Abstract
- Keywords
- Resumen
- Palabras clave
- Introduction
- Methods
- Methodology
- Protocol
- Statistical analyses
- Results
- Discussion
- Conclusion
- Conflict of interest
- Bibliography
 Tables (3) Table 1. Baseline Demographic Characteristics, Comorbidities, and Medical Treatment Received Before Allocation to Treatment.
Tables (3) Table 1. Baseline Demographic Characteristics, Comorbidities, and Medical Treatment Received Before Allocation to Treatment. 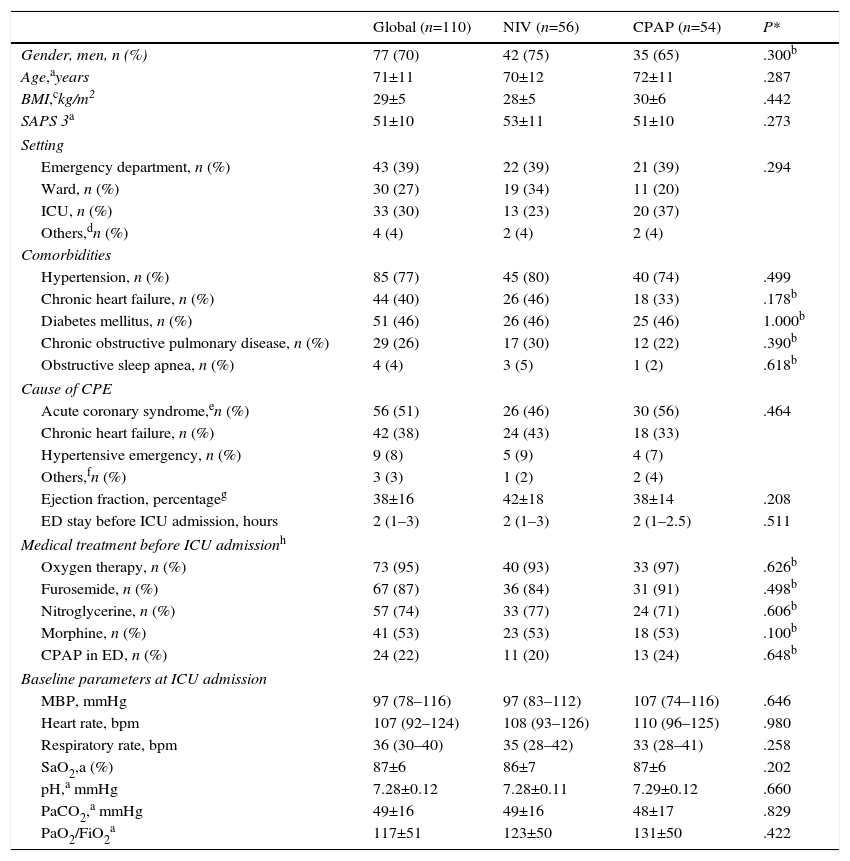 Table 2. Analysis of Primary and Secondary Outcomes of the Study.
Table 2. Analysis of Primary and Secondary Outcomes of the Study. 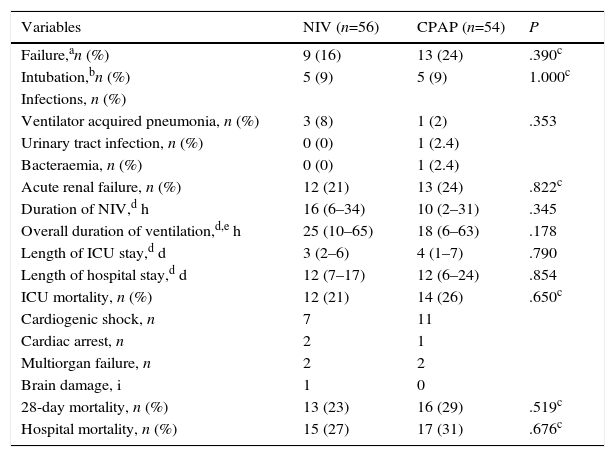 Table 3. Analysis of primary and secondary outcomes in the hypercapnic group.
Table 3. Analysis of primary and secondary outcomes in the hypercapnic group. 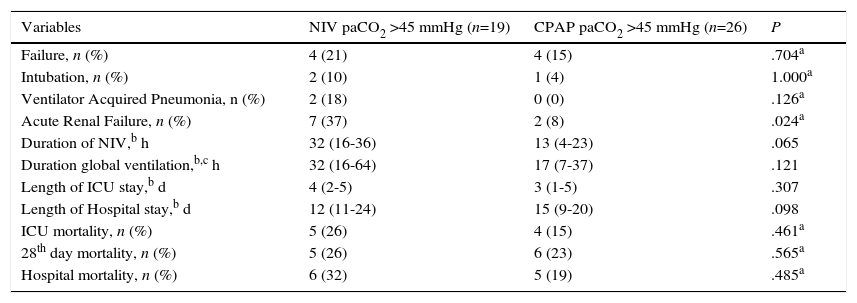 AbstractBackground
AbstractBackgroundTo compare the application of non-invasive ventilation (NIV) versus continuous positive airway pressure (CPAP) in the treatment of patients with cardiogenic pulmonary edema (CPE) admitted to an intensive care unit (ICU).
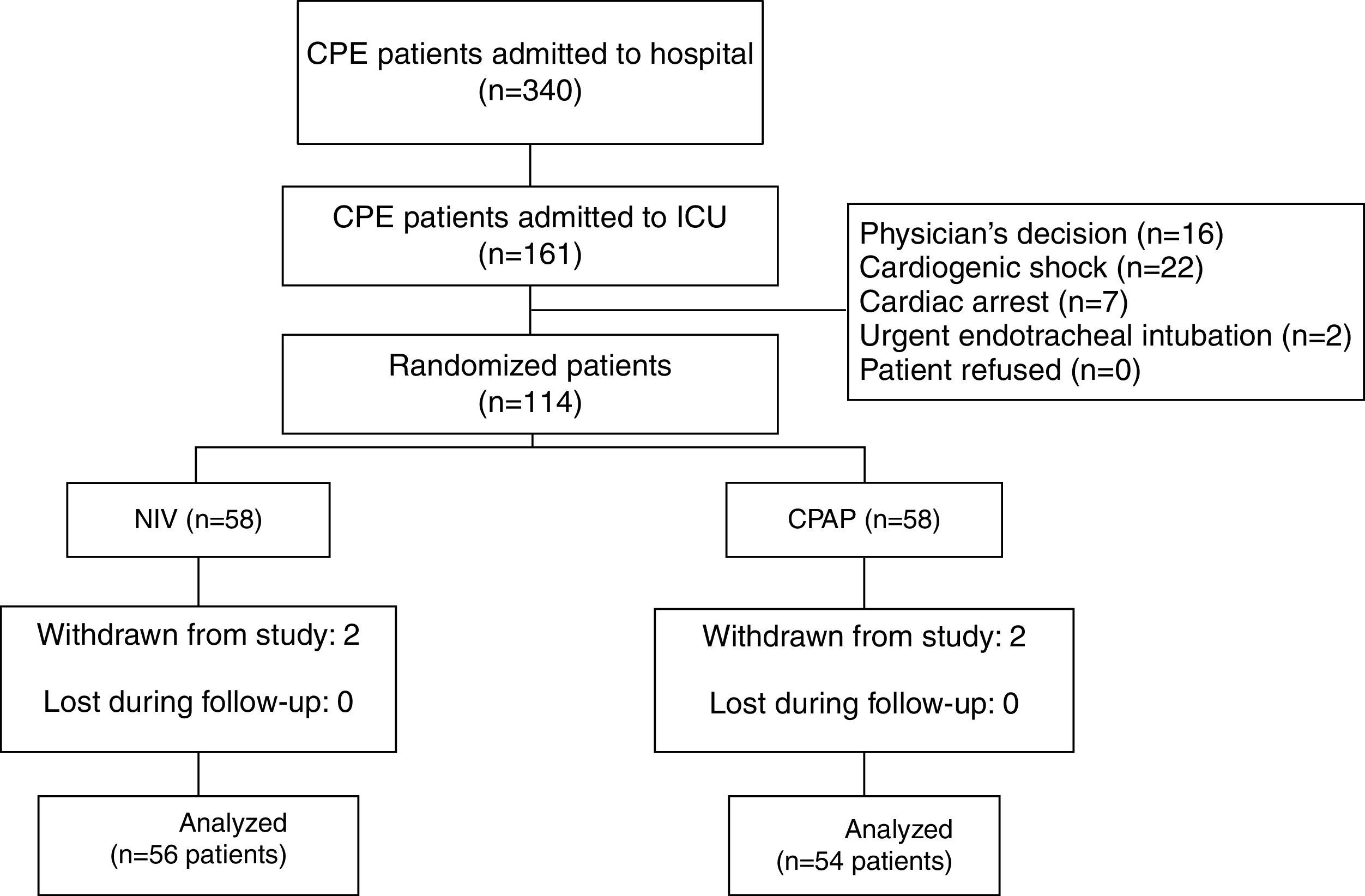
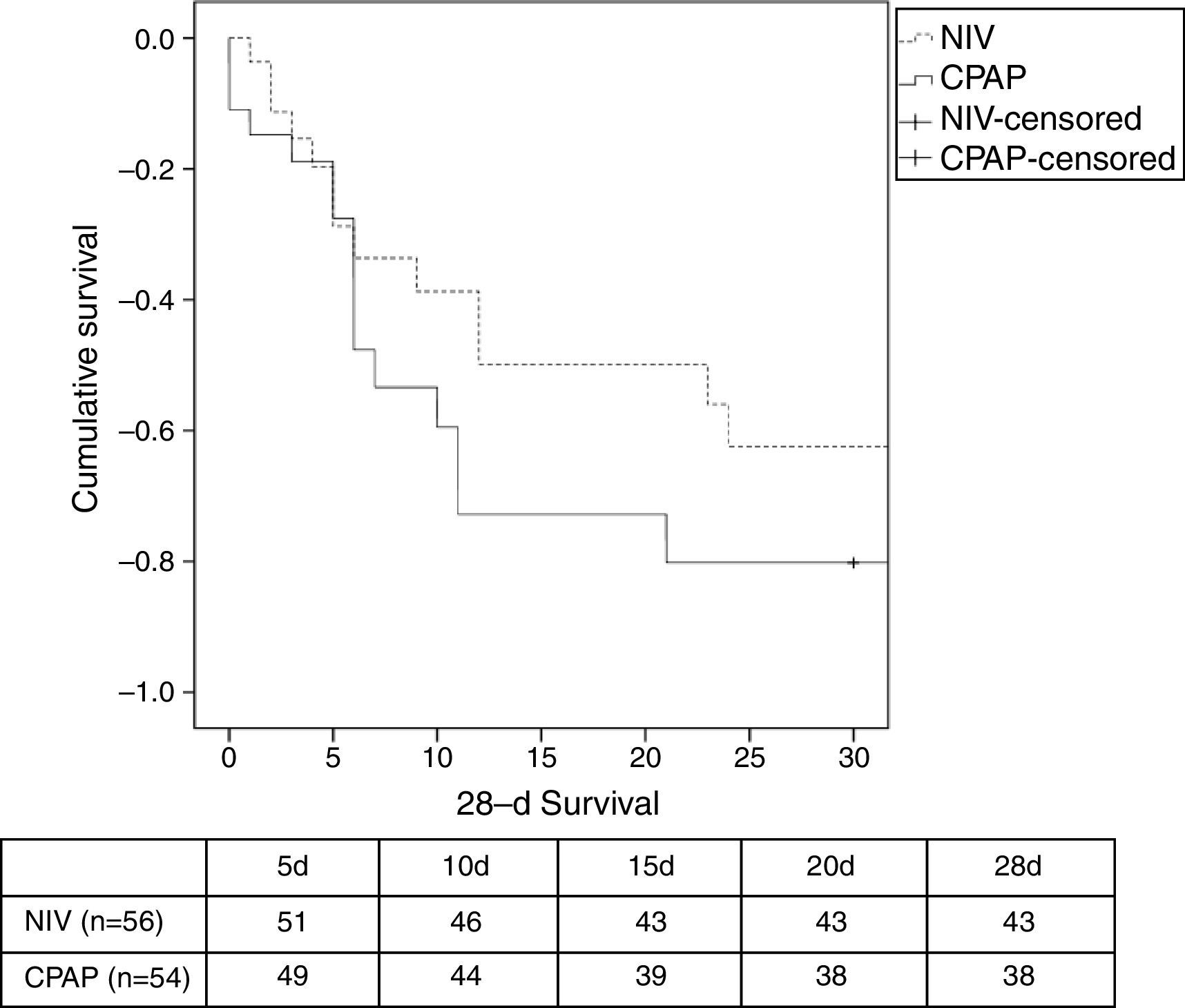
MethodsIn a prospective, randomized, controlled study performed in an ICU, patients with CPE were assigned to NIV (n=56) or CPAP (n=54). Primary outcome was intubation rate. Secondary outcomes included duration of ventilation, length of ICU and hospital stay, improvement of gas exchange, complications, ICU and hospital mortality, and 28-day mortality. The outcomes were analyzed in hypercapnic patients (PaCO2>45mmHg) with no underlying chronic lung disease.
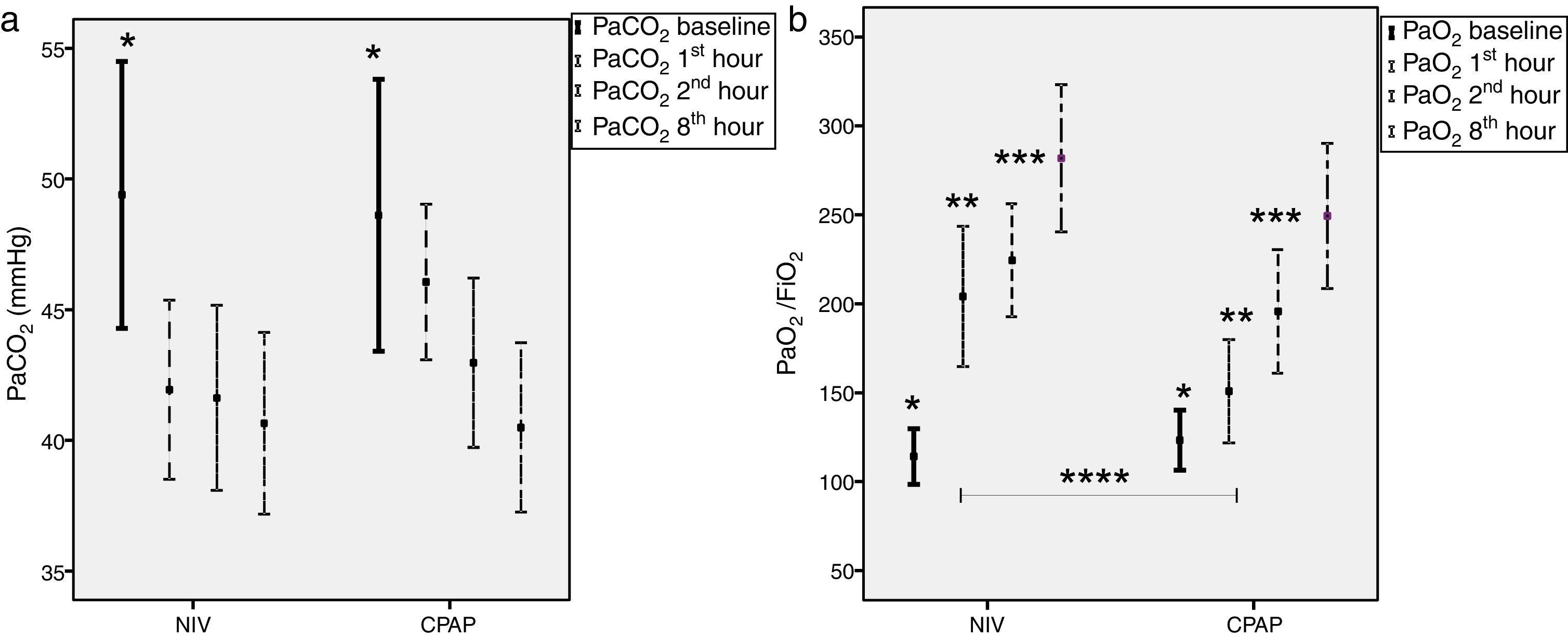
ResultsBoth devices led to similar clinical and gas exchange improvement; however, in the first 60min of treatment a higher PaO2/FiO2 ratio was observed in the NIV group (205±112 in NIV vs. 150±84 in CPAP, P=.02). The rate of intubation was similar in both groups (9% in NIV vs. 9% in CPAP, P=1.0). There were no differences in duration of ventilation, ICU and length of hospital stay. There were no significant differences in ICU, hospital and 28-d mortality between groups. In the hypercapnic group, there were no differences between NIV and CPAP.
ConclusionsEither NIV or CPAP are recommended in patients with CPE in the ICU. Outcomes in the hypercapnic group with no chronic lung disease were similar using NIV or CPAP.
Keywords:Noninvasive ventilationContinuous positive airway pressureCardiogenic pulmonary edemaAcute respiratory failureResumenIntroducciónComparar la efectividad de la ventilación no invasiva (VNI) frente a la presión positiva continúa en la vía aérea (CPAP) en pacientes ingresados por edema agudo de pulmón (EAP) cardiogénico en una unidad de cuidados intensivos (UCI).
MétodosEnsayo clínico donde 56 pacientes fueron asignados a VNI y 54 pacientes a CPAP. El objetivo primario fue la tasa de intubación. Los objetivos secundarios fueron: duración de ventilación, estancia en UCI y en el hospital, mejoría gasométrica, complicaciones y mortalidad en UCI, hospitalaria y a los 28 días. Los objetivos fueron analizados en pacientes hipercápnicos (PaCO2 >45mmHg) sin patologia pulmonar.
ResultadosAmbos dispositivos obtuvieron similar mejoría clínica y del intercambio gaseoso, sin embargo, la VNI mostró un aumento más rápido de la oxigenación (medido por el cociente PaO2/FiO2) en los primeros 60 minutos de aplicación (205±112 en VNI vs. 150±84 en CPAP, p= 0,02). La tasa de intubación fue similar en ambos grupos (9% en VNI vs. 9% en CPAP, p= 1,0). No hubo diferencias en la duración de la ventilación, ni en la estancia en UCI ni hospitalaria. Tampoco hubo diferencias significativas en la mortalidad en UCI, hospitalaria y a los 28 días entre ambos grupos. En el subgrupo de pacientes hipercápnicos tampoco se observaron diferencias significativas en los objetivos analizados.
ConclusionesLa VNI como la CPAP se pueden emplear en pacientes con EAP en la UCI. En pacientes hipercápnicos sin patología pulmonar no se observa beneficio de la VNI sobre la CPAP.
Palabras clave:Ventilación no invasivaPresión positiva continua en la vía aéreaEdema agudo de pulmón cardiogénicoInsuficiencia respiratoria aguda Full Text IntroductionCardiogenic pulmonary edema (CPE) is a cause of hypoxemic acute respiratory failure (ARF) due to acute heart failure. Traditionally, the standard medical treatment for CPE has been morphine, nitroglycerin, oxygen therapy and diuretics, and endotracheal intubation.1
Development of ventilatory support devices, such as continuous positive airway pressure (CPAP) and non-invasive ventilation (NIV), has played a decisive role in the treatment of ARF secondary to CPE. The use of either CPAP2–7 or NIV8–11 has resulted in greater clinical improvements compared with standard medical therapy. Hypercapnia without chronic lung disease has been associated with poor outcomes in patients with CPE,12,13 particularly when PaCO2 is higher than 60mmHg.13 Although there is a strong indication for NIV in hypercapnic patients,11,12 the superiority of NIV over CPAP remains unclear, and hence, both have been recommended.14–31
NIV and CPAP have both been successfully used in CPE patients admitted to an intensive care unit (ICU).8–10,28 However, few trials have been published in the ICU setting.10,28 In addition, acute coronary syndrome (ACS) has been considered to be an exclusion criterion in several trials.10,11,18,19,28–31
The aim of the present study was to demonstrate that NIV performs better than CPAP in the management of CPE in an ICU setting. The primary outcome was a reduction in the need for endotracheal intubation in the NIV group. The secondary outcomes were duration of ventilation, ICU and hospital stay, ICU and hospital mortality, and 28-day mortality. The clinical and gasometric improvements, together with the rate of complications (renal failure, nosocomial infections), were all recorded. We also assessed the role of hypercapnia (PaCO2>45mmHg) on primary and secondary outcomes in patients with no underlying chronic lung disease.
MethodsA prospective, randomized study was conducted in a medical-surgical ICU from July 2007 to December 2010. The study protocols were approved by the local clinical research ethics committee. Written consent was required from all patients, or from their next of kin, before inclusion in the study. CPE patients aged 18 years or older admitted to the ICU from the emergency department (ED), a hospital ward, or the cardiac catheterization laboratory were included in the study. Cardiogenic pulmonary edema is defined as the presence of dyspnea, respiratory rate >25breaths/minute, the use of accessory respiratory muscles, cyanosis, cold sweats, bilateral crackles and/or wheezing on pulmonary auscultation, hypoxemia, hypertension, and a predominance of bilateral pulmonary infiltrates on chest radiography (if available).1 The potential causes of CPE are understood to be ACS with or without persistent ST-elevation, hypertensive emergency, valvulopathy, acute arrhythmia, endocarditis, or decompensation due to chronic heart failure.1 The exclusion criteria were: refusal to give informed consent, inability to cooperate, severe encephalopathy (Glasgow coma score 45mmHg.11,13 Patients with chronic obstructive pulmonary disease (COPD) or obstructive sleep apnea syndrome (OSA) were excluded for the analysis in the hypercapnic group.
MethodologyPatients were continuously monitored via electrocardiography and invasive or non-invasive blood pressure measurements. Blood oxygen was monitored using pulse oximetry, which estimates transcutaneous arterial oxygen saturation (SaO2), together with arterial blood samples for ABG analyses using the ABL 800 Flex (Radiometer™, Denmark, Copenhagen) blood gas analyzer which measures partial pressure of oxygen (PaO2), PaCO2, partial pressure of oxygen to fraction of oxygen ratio (PaO2/FiO2), and pH. Demographic data, comorbidities, and predicted mortality using the Simplified Acute Physiology Score 3 (SAPS 3), were all collected on admission. All vital signs and arterial blood gases (if available) were recorded at baseline and at 1, 2 and 8h after randomization. All complications arising during ICU stay were recorded, and patients were followed up for 28 days or until hospital discharge.
At the time of onset of CPE, either in the ED or on the ward, all patients received standard medical therapy (oxygen through a Venturi mask, morphine, intravenous nitroglycerin if SBP >160mmHg, together with loop diuretics) at the discretion of the attending physician. In the absence of clinical improvement (dyspnea, respiratory rate >25bpm, SaO2
Tag » What Is A Non-continuous Ventilator
-
21 CFR § 868.5905 - Noncontinuous Ventilator (IPPB).
-
Non Continuous Ventilator - An Overview | ScienceDirect Topics
-
Philips Respironics Recalls Certain Continuous And Non ... - FDA
-
Phillips Continuous & Non-Continuous Ventilator Recall
-
Non-invasive Ventilation - Wikipedia
-
Non Invasive Ventilation - Physiopedia
-
BZD Ventilator, Non-Continuous (Respirator) - PathSurveyor
-
The Difference Between CPAP, BiPAP, And Ventilators
-
Ventilators - FDA Regulatory Consulting And Training Services
-
What Is Continuous Positive Airway Pressure (CPAP)? - Medmastery
-
Philips Respironics Recall Of Positive Airway Pressure And ...
-
Continuous Positive Airway Pressure - StatPearls - NCBI Bookshelf
-
Non-Invasive Ventilation Versus Continuous Positive Airway ...
-
Continuous Positive Airway Pressure (CPAP) Non-invasive Ventilation