Human Spine And Spinal Cord C1 To S5 Vertebra - Disabled World
Author: Ian C. Langtree - Writer/Editor for Disabled World (DW)Published: 2017/12/01 - Updated: 2024/09/23Publication Type: InformativeCategory Topic: Spinal Cord Injury - Related Publications
Page Content: Synopsis - Introduction - Main
Synopsis: The information below provides a comprehensive overview of the human spine and spinal cord, detailing the structure and function of each vertebra from C1 to S5. This knowledge is important for understanding spinal cord injuries (SCIs) and their potential impacts on various body functions. The resource explains how injuries at different levels of the spine can affect mobility, sensation, and autonomic functions, which is valuable for medical professionals, patients, and caregivers in comprehending the consequences of SCIs and planning appropriate care and rehabilitation strategies. By providing detailed descriptions of each vertebra and associated nerves, the information aids in the accurate diagnosis and treatment of spinal conditions, ultimately contributing to better patient outcomes and quality of life for those affected by spinal cord injuries or disorders - Disabled World (DW).
Defining Spinal Cord Injury (SCI)
Spinal Cord Injury (SCI)A spinal cord injury (SCI) is damage to the tight bundle of cells and nerves that sends and receives signals from the brain to and from the rest of the body. The spinal cord extends from the lower part of the brain down through the lower back. An SCI can occur anywhere along the spinal cord. It is the result of damage to cells in the spinal cord and causes a loss of communication between the brain and the parts of the body below the injury. Effects of an SCI may include low blood pressure, inability to regulate blood pressure effectively, reduced control of body temperature, inability to sweat below the level of injury, and chronic pain.
A spinal cord injury can be classified by into two types: complete or incomplete:
- A complete injury means that there is no nerve communication below the injury site; sensory and motor function below this site is lost.
- An incomplete injury means the spinal cord is still able to transmit some messages to or from the brain. People with incomplete injuries retain some sensory function and may have some control of muscle activity below the injury site.
Introduction
The human spinal cord consists of nerves that connect the brain to nerves in the body. It is a superhighway for messages between the brain and the rest of the body. The spinal cord is surrounded for most of its length by the bones (vertebrae) that form the spine.
Main Content
The outer layer of the human spinal cord consists of white matter, i.e., myelin-sheathed nerve fibers. These are bundled into specialized tracts that conduct impulses triggered by pressure, pain, heat, and other sensory stimuli or conduct motor impulses activating muscles and glands. The inner layer, or gray matter, is mainly composed of nerve cell bodies. Within the gray matter, running the length of the cord and extending into the brain, lies the central canal through which the cerebrospinal fluid circulates.
How Long is the Spinal Cord?
- The human spinal cord, part of the central nervous system, is around 45 cm (18 in) in men and around 43 cm (17 in) long in women. The spinal cord has a varying width, ranging from 13 mm (1/2 in) thick in the cervical and lumbar regions to 6.4 mm (1/4 in) thick in the thoracic area. Your spinal cord is protected by the vertebral column (spinal column or backbone).
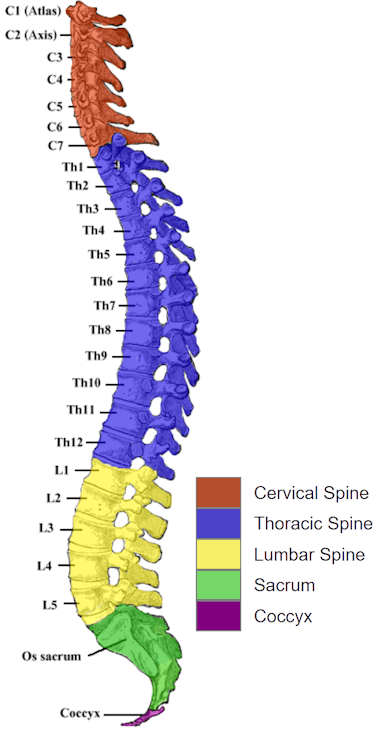
How Many Bones Constitute the Human Spine?
- The human spinal column is made up of 33 bones - 7 vertebrae in the cervical region, 12 in the thoracic region, 5 in the lumbar region, 5 in the sacral region and 4 in the coccygeal region.
What is the Difference Between Vertebrates and Invertebrates?
- Vertebrates have a backbone or a spinal column.
- Invertebrates do not have a backbone or a spinal column.
What is the Difference Between Vertebra and Vertebrae?
- Vertebra = Singular
- Vertebrae = Plural
Spinal Cord Injury Information on Vertebra C1 to S5
- Jump To:
- Cervical (C1 - C8)
- Thoracic (T1 - T12)
- Lumbar (L1 - L5)
- Sacral (S1 - S5)
C1 C2 C3 C4 C5 C6 C7 C8 T1 T2 T3 T4 T5 T6 T7 T8 T9 T10 T11 T12 L1 L2 L3 L4 L5 S1 S2 S3 S4 S5
Cervical (neck) Injuries (C1 to C8)
C1 - Atlas
The Atlas is the topmost vertebra, and along with C2, forms the joint connecting the skull and spine. Its chief peculiarity is that it has no body, and this is because the body of the atlas has fused with that of the next vertebra.
C2 - Axis
Forms the pivot upon which C1 rotates. The most distinctive characteristic of this bone is the strong odontoid process (dens) which rises perpendicularly from the upper surface of the body. The body is deeper in front than behind, and prolonged downward anteriorly to overlap the upper and front part of the third vertebra. Injuries to C-1 and C-2 can result in a loss of many involuntary functions including the ability to breathe, necessitating breathing aids such as ventilators or diaphragmatic pacemakers.
C3
Injury to spinal bone three often causes pain, tingling, and sometimes numbness in the arms, neck, and head. If the fourth cervical vertebrae (C4) nerve root is also involved, pain is usually felt in the upper arms and shoulders, as well as the lower neck.
C4
Cervical Vertebra - Quadriplegia and breathing difficulty - The fourth cervical (neck) vertebra from the top. Injuries above the C-4 level may require a ventilator for the person to breathe properly.
C5
Quadriplegia with some shoulder and elbow function - 5th cervical vertebrae down from the base of the skull, found in the neck. C5 injuries often maintain shoulder and biceps control, but have no control at the wrist or hand.
- C5 to C8 injuries
Corresponding nerves control the arms and hands, a person with this level of spinal injury may still be able to breathe on their own and speak normally.
C6 - Cervical Vertebra
Quadriplegia with shoulder, elbow, and some wrist function - The sixth cervical (neck) vertebra from the top. The next-to-last of the seven cervical vertebrae. An injury to the spinal cord between C6 and C7 vertebrae is called a C6-7 injury. These injuries generally allow wrist control, but no hand function.
C7 - Vertebra Prominens
Quadriplegia with shoulder, elbow, wrist, and some hand function - The most distinctive characteristic of this vertebra is the existence of a long and prominent spinous process, hence the name vertebra prominens. In some subjects, the seventh cervical vertebra is associated with an abnormal pair of ribs, known as cervical ribs. These ribs are usually small, but may occasionally compress blood vessels (such as the subclavian artery) or nerves in the brachial plexus, causing unpleasant symptoms. C-7 and T-1 can straighten their arms, but still may have dexterity problems with the hand and fingers. Injuries at the thoracic level and below result in paraplegia, with the hands not affected.
C8
Quadriplegia with normal arm function; hand weakness - Although there are seven cervical vertebrae (C1-C7), there are eight cervical nerves (C1-C8). All nerves except C8 emerge above their corresponding vertebrae, while the C8 nerve emerges below the C7 vertebra. In other words, C8 is a nerve root, not vertebrae.
SCI Summary - C1 to C8
- Most severe of the spinal cord injury levels.
- C2 to C3 - Usually fatal as a result of inability to breathe.
- Requires 24 hour a day assistance.
- Paralysis in arms, hands, trunk, and legs.
- Will not be able to drive a car on their own.
- Ability to speak is sometimes impaired or reduced.
- If both arms and legs are affected, this is called tetraplegia or quadriplegia.
- May be able to use powered wheelchairs with special controls to move around on their own.
- Patient may not be able to breathe on his or her own, cough, or control bowel or bladder movements.
- Requires complete assistance with activities of daily living, such as eating, dressing, bathing, and getting in or out of bed.
Thoracic Vertebrae (T1 to T12)
T1
Comparatively speaking, T1 is the smallest of all thoracic vertebrae. The T1 vertebra is the first (uppermost) of the twelve (12) thoracic vertebrae that make up the central and largest section of the spinal column between the lumbar vertebrae below and the cervical vertebrae above.
T2
The second vertebra in the thoracic spine is responsible for helping to support the rib cage. The T2 vertebra possesses facets that create joints with two of the ribs, thus helping to keep the thoracic spine far more stable than the cervical spine in the neck or the lumbar spine in the lower back. T2 vertebra degeneration includes: Herniated, bulging or prolapsed discs, Bone spurs, Facet disease, forms of osteoarthritis and Traumatic or sports-related injuries.
T3
The third thoracic vertebrae is a small vertebra in the upper middle back that plays an integral role in supporting the rib cage. The anterior aspect of the upper thoracic spine is a difficult region to approach in spinal surgery.
T4
Spinal cord transection at T4 results in severe damage to the nervous tissue, with impairment of motor, sensory and autonomic functions. T4 syndrome is a relatively uncommon condition in which spinal injury at the T4 vertebra causes a set of symptoms including diffuse arm pain and pins and needles or numbness in the upper arm.
T5
The T5 vertebra, as well as the rest of the thoracic spine, provides a stable foundation for the human rib cage.
T6
An injury at the level of T6 (thoracic) spinal cord results in damage to the autonomic nervous system, both the sympathetic and parasympathetic divisions, affecting the function of major abdominal organs.
T7
The T7 vertebra is in the middle of the twelve (12) thoracic vertebrae of the torso and the center of the spinal column. Thoracic vertebrae play an important role, not only in the protection of the spinal cord, but also in the protection of vital organs. A vertebral compression fracture refers to a break of the vertebral body, most often below the T7 level of the thoracic spine (upper back), and is most commonly caused by weakened bone resulting from osteoporosis. Most vertebral compression fractures result in a loss of more than 15% to 20% of the height of the vertebra.
T8
T8 vertebra is toward the lower (caudal) end of the twelve (12) thoracic vertebrae within the central, torso section of the spine. Like other spinal vertebrae, the T8 primarily protects and encases the spinal cord. The T8 is also at the same level as the xiphoid process. The eighth thoracic spinal nerve runs beneath the T8. Throughout the thoracic spine, discs like those above and beneath the T8 vertebra can become damaged and cause painful symptoms.
T9
T9 to T12 are known as the transition vertebrae. The lumbar cord is situated between T9 and T11 vertebrae. T9 to T12 injuries can be classified as either complete or incomplete injuries. Complete injuries result in the total loss of movement and sensation below the point of injury, while incomplete injuries indicate that some function below the level of injury is retained.
T10
T10 is situated at the umbilicus. The T10 vertebra is near the bottom of the twelve (12) thoracic vertebrae (T1-T12) within the torso and making up the central portion of the spinal column. This particular vertebra has a complete articular facet and the thoracic spinal nerves passes out under it. T10 innervates the muscles of the lower abdomen. It is part of the section of the spinal cord which is most vulnerable to injury due to the area's high level of flexibility. An injury in this area will most likely experience limited or complete loss of use of the muscles in the lower abdomen, buttocks, legs, and feet. The extent of disability is determined by damage done to the T10 vertebra. Partial damage may cause weakness, numbness, lack of muscle control, or loss of the use of one side of the lower body. Complete damage could result in the loss of use of the lower body (paraplegia).
T11
The ribs connected to T11 and T12 at the bottom of the thoracic spine do not attach the sternum in front, but do provide protection for the kidneys in the back of the body. Because these levels have slightly less stability, they are slightly more prone to problems that can cause pain. A person with a T11 vertebral injury may have or recover sensations in the L1 through L4 dermatomes, which include the front of the leg down to the mid-shin level. In addition, such a patient should recover hip extensors, knee extensors, and even ankle dorsiflexion. However, the sacral functions, including bowel and bladder and many of the flexor functions of the leg may be absent or weak.
T12
T12 ends just above the hip girdle. T12 bears the most weight of any thoracic vertebra, making it the strongest thoracic vertebra, but also the most susceptible to stress-related injuries. Compression fractures of the spine usually occur at the bottom part of the thoracic spine (T11 and T12) and the first vertebra of the lumbar spine (L1). The most common thoracic spinal cord injury involves T11 and T12.
SCI Summary - T1 to T12
The thoracic vertebrae increase in size from T1 through T12 and represent the 12 thoracic vertebrae. The thoracic vertebrae are situated between the cervical (neck) vertebrae and the lumbar vertebrae. These thoracic vertebrae provide attachment for the ribs and make up part of the back of the thorax or chest. Damage or SCI's above the T1 vertebra affects the arms and the legs. Injuries below the T1 vertebra affect the legs and trunk below the injury, but usually do not affect the arms and hands. Paralysis of the legs is called paraplegia. Paralysis of the arms AND legs is called quadriplegia.
The most common fractures of the spine occur in the thoracic (mid-back) and lumbar spine (lower back) or at the connection of the two (thoracolumbar junction). These fractures are typically caused by high-velocity accidents, such as a car crash, or a fall from a height.
- T1 to T6:
Paraplegia with loss of function below mid-chest; full control of arms
- T1 to T8:
Most often control the hands, but poor trunk control as the result of lack of abdominal muscle control.
- T6 to T12:
Paraplegia with loss of function below the waist; good control of torso
- T9 to T12:
Allow good trunk control and abdominal muscle control. Lumbar and Sacral injuries yield decreasing control of the hip flexors and legs. Individuals with SCI also experience other changes. For example, they may experience dysfunction of the bowel and bladder.
- Corresponding nerves affect muscles, upper chest, mid-back and abdominal muscles.
T1 to T5 Thoracic Nerves:
- Can learn to drive a modified car.
- Arm and hand function is usually fairly normal.
- Will most likely need to use a manual wheelchair.
- Injuries usually affect the trunk and legs (paraplegia).
- Can stand with the use of a standing frame, some patients may walk with braces
T6 to T12 Thoracic Nerves:
- Nerves affect muscles of the trunk (abdominal and back muscles) depending on the level of injury.
- Usually results in paraplegia.
- Normal upper-body movement.
- Can learn to drive an adapted vehicle.
- Most likely will need to use a manual wheelchair.
- Should be able to cough productively (if abdominal muscles are intact).
- A fair to good ability to control and balance the body while in a seated position.
- Some patients will be capable of standing in a standing frame, while others may require the use of braces to walk.
- Often will have little or no voluntary control of bowel or bladder function, but can usually manage on their own with adaptive equipment.
Lumbar Vertebrae (L1 to L5)
L1
The first lumbar vertebra is at the same level as the ninth rib. This level is also called the important transpyloric plane, since the pylorus of the stomach is at this level.
L2
Injuries to the spinal column at L2 or lower will damage the tip of the spinal cord, called the conus, or the spray of spinal roots that are descending to the appropriate spinal vertebral levels to exit the spinal canal or the caudal equina.
L3
The L3 vertebra is in the middle of the five lumbar vertebrae in the lower back portion of the spinal column. The L3 vertebra, or third lumbar vertebra, is one of the most common sites for the occurrence of a herniated disc and other spinal conditions that can cause chronic lower back pain. A lot of motion in the back is divided between these five motion segments, with segments L3 - L4 and L4 - L5 taking most of the stress. L3 - L4 and L4 - L5 segments are most likely to breakdown from wear and tear, causing such conditions as osteoarthritis. L2 and L3 cover the front part of the thighs.
L4
The most likely to herniate. The effects of this can cause pain and numbness that can radiate through the leg and extend down to the feet (sciatica). Spondylolysis and spondylolisthesis are conditions that affect the moveable joints of the spine that help keep the vertebrae aligned one on top of the other. Spondylolysis is actually a weakness or stress fracture in one of the bony bridges that connects the upper and lower facet joints. This fracture can happen at any level of the spine, but usually occurs at the fourth (L4) or fifth (L5) lumbar vertebra. L4 and L5 fractures are commonly the result of a high-impact trauma from falls or motor vehicle accidents.
L5
The fifth lumbar vertebra (L5) is the largest of the five lumbar vertebrae and is considered an atypical vertebra due to its shape. As the last of the lumbar vertebrae, the L5 vertebra bears more body weight than any of the other 23 vertebrae that sit atop it in the vertebral column. The L4 and L5 disc, in between the L4 and L5 vertebrae, can herniate or degenerate, leading to possible leg pain (sciatica) or lower back pain. The fifth lumbar vertebra is the most common site of spondylolysis and spondylolisthesis. Sacral Nerves (S1 to S5) injuries generally result in some loss of functionin the hips and legs. Little or no voluntary control of bowel or bladder, but patients can manage on their own with special equipment. Most likely, they will also still be able to walk.
SCI Summary - L1 to L5
Lumbar nerves (L1 to L5) injuries generally result in some loss of function in the hips and legs. Often there is little or no voluntary control of bowel or bladder, but patients usually manage on their own with the use of special equipment. Depending on strength in the legs, some patients may need a wheelchair and may also walk with braces.
The lumbar vertebrae graduate in size from L1 through L5. These vertebrae bear much of the body's weight and related biomechanical stress. The lumbar vertebrae are also the largest segments of the movable part of the vertebral column, and are characterized by the absence of the foramen transversarium within the transverse process, and by the absence of facets on the sides of the body. Some individuals have four lumbar vertebrae, while others have six. Lumbar disorders that normally affect L5 will affect L4 or L6 in these individuals.
Sacral Nerves (S1 to S5)
The sacrum is shaped different in males and females. In females, the sacrum is shorter and wider than in males. The Sacrum is located behind the pelvis. Five bones (abbreviated S1 through S5) fused into a triangular shape, form the sacrum. The sacrum fits between the two hipbones connecting the spine to the pelvis, located just below the lumbar vertebrae.
The Sacrum consists of four or five sacral vertebrae in a child, which become fused into a single bone after age 26. The sacrum forms the back wall of the pelvic girdle and moves with it.
The first three vertebrae in the sacral have transverse processes which come together to form wide lateral wings called alae. These alae articulate with the blades of the pelvis (ilium).
As part of the pelvic girdle, the sacrum forms the back wall of the pelvis and also forms joints at the hip bone called the sacroiliac joints. The sacrum contains a series of four openings on each side, through which the sacral nerves and blood vessels run. The sacral canal runs down the center of the sacrum and represents the end of the vertebral canal.
Back pain or leg pain (sciatica) can typically arise due to injury where the lumbar spine and sacral region connect (at L5 - S1) because this section of the spine is subjected to a large amount of stress and twisting.
People with rheumatoid arthritis or osteoporosis are inclined to develop stress fractures and fatigue fractures in the sacrum.
The bottom of the spinal column is called the coccyx or tailbone. It consists of 3 to 5 bones that are fused in an adult. Many muscles connect to the coccyx.
Sacral Nerves (S1 to S5) injuries generally result in some loss of function in the hips and legs. Little or no voluntary control of bowel or bladder, but can manage on their own with special equipment. Most likely will be able to walk.
S1
- L5 to S1 Isthmic Spondylolisthesis:
A small fracture in the facet joints can allow the L5 vertebra to slip forward over the S1 vertebra, impinging the nerve root and leading to leg pain and other symptoms.
- L5-S1 disc herniation:
Occurs when the inner portion leaks out and touches the nearby nerve root, causing pain to radiate in the lower back or down the leg.
- L5-S1 degenerative disc disease:
If the L5-S1 disc is compromised, the L5-S1 disc itself can become a source of lower back or leg pain.
S2
S2 is located at the level of posterior superior iliac spine. S2 covers the back of the thighs.
S3
S3 cover the medial side of the buttocks.
S4
S4-5 covers the perineal region.
S5
S5 is the lowest dermatome and represents the skin immediately at and adjacent to the anus.
This chart is a general guide only; impairments and rehabilitation varies greatly depending on type and severity of SCI.
 Author Credentials: Ian is the founder and Editor-in-Chief of Disabled World, a leading resource for news and information on disability issues. With a global perspective shaped by years of travel and lived experience, Ian is a committed proponent of the Social Model of Disability-a transformative framework developed by disabled activists in the 1970s that emphasizes dismantling societal barriers rather than focusing solely on individual impairments. His work reflects a deep commitment to disability rights, accessibility, and social inclusion. To learn more about Ian's background, expertise, and accomplishments, visit his full biography.
Author Credentials: Ian is the founder and Editor-in-Chief of Disabled World, a leading resource for news and information on disability issues. With a global perspective shaped by years of travel and lived experience, Ian is a committed proponent of the Social Model of Disability-a transformative framework developed by disabled activists in the 1970s that emphasizes dismantling societal barriers rather than focusing solely on individual impairments. His work reflects a deep commitment to disability rights, accessibility, and social inclusion. To learn more about Ian's background, expertise, and accomplishments, visit his full biography.
Từ khóa » C1-c7 T1-12
-
Spinal Anatomy | Vertebral Column - SpineUniverse
-
Spinal Anatomy Center | Cervical, Thoracic, And Lumbar Spine Info
-
Normal Spinal Anatomy - Spine-health
-
All About The C7-T1 Spinal Segment (Cervicothoracic Junction)
-
Regions Of The Spine - Cervical, Thoracic, Lumbar, Sacral
-
Regions Of The Spine » SONSA
-
Spine Anatomy
-
The Anatomy Of Your Spine: What You Need To Know
-
Anatomy Of The Spine And Peripheral Nervous System
-
Spine Anatomy: Image Details - NCI Visuals Online
-
The Vertebral Column | Anatomy And Physiology I - Lumen Learning
-
Spine Anatomy - The Brain And Spine Clinic
-
The Spine: Support System For The Body | Minster Chiropractic Center