ACTINOMYCES AND NOCARDIA Do Dr Hrisi BAHAR ...
Có thể bạn quan tâm
ACTINOMYCES AND NOCARDIA Doç. Dr. Hrisi BAHAR
ACTINOMYCETES
AEROBIC ACTINOMYCETES ► Gram-positive branching filaments that sporulate or fragment: According to the composition of the cell wall they are studied in 2 groups. ► 1 - Aerobic Actinomycetes whose cell walls contain mycolic acid: Nocardia species and Rhodococcus species ► 2 -Aerobic Actinomycetes whose cell walls lack mycolic acid: Streptomyces species
ANAEROBIC ACTINOMYCETES ► Anaerobic non-sporulating Gram- positive rods consist of two groups based on guanosine (G) plus cytosine (C) DNA content: 1 -Low mole percent (30 -53%) 2 -High mole percent (49 -68%) ► Actinomyces species are member of the high G+C group.
Pathogenic Genera of Aerobic Actinomycetes ► Nocardia ► Actinomadura ► Streptomyces ► Rhodococcus ► Gordonia ► Tsukamurella ► Tropheryma whipplei (Non-cultivable)
Aerobic Actinomycetes: Natural Habitats n n n Nocardia species and other aerobic Actinomycetes are in soil and primarily responsible for decomposition of organic plant matter Rhodococcus species present in the intestinal bacterial flora of grazing herbivores especially horses Streptomyces species (>3, 000) widely distributed in soil
Anaerobic Actinomycetes: Natural Habitats Anaerobic Actinomyces species are normal inhabitants of the mucous membranes of humans and animals
Aerobic Actinomycetes: Modes of Infection ► Actinomadura species (A. madurae, A. latina, A. pelletieri) produce subcutaneous infections in tropical and subtropical countries with those who walk barefooted ► Gordonia and Tsukamurella species are closely related to Rhodococcus, and are soil organisms considered opportunistic pathogens
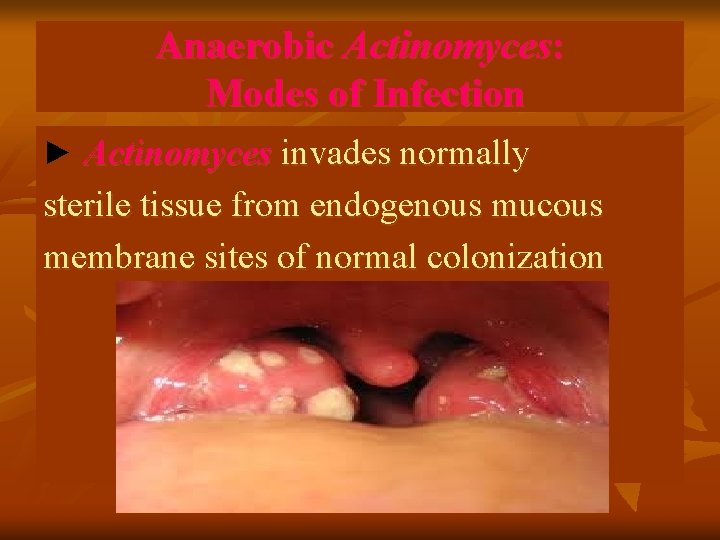
Anaerobic Actinomyces: Modes of Infection ► Actinomyces invades normally sterile tissue from endogenous mucous membrane sites of normal colonization
Aerobic Actinomycetes: Types of Infectious Disease -1► Rhodococcus equi infects macrophages inhibiting phagolysosome fusion, and produces pulmonary disease with cavitation. Infection occurs in immunocompromised (especially HIV-infected) individuals who handle horses. ► R. equi disseminates to other organs including the brain and subcutaneous tissue
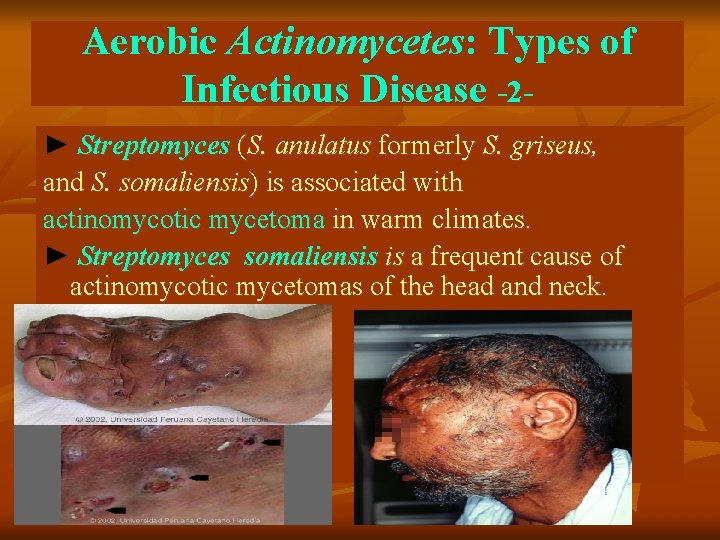
Aerobic Actinomycetes: Types of Infectious Disease -2► Streptomyces (S. anulatus formerly S. griseus, and S. somaliensis) is associated with actinomycotic mycetoma in warm climates. ► Streptomyces somaliensis is a frequent cause of actinomycotic mycetomas of the head and neck.
Aerobic Actinomycetes: Types of Infectious Disease ► Whipple’s disease: The cause is infection with the bacterium Tropheryma whipplei. This bacterium can initially affect the mucosal lining of the small intestine, forming small lesions within the intestinal wall. With time, the infection can spread to other parts of the body. Diarrhea, weight loss, lymphadenopathy, fever, and arthralgia are between the symptoms ► Diagnosis is by typical histopathology combined with PCR)
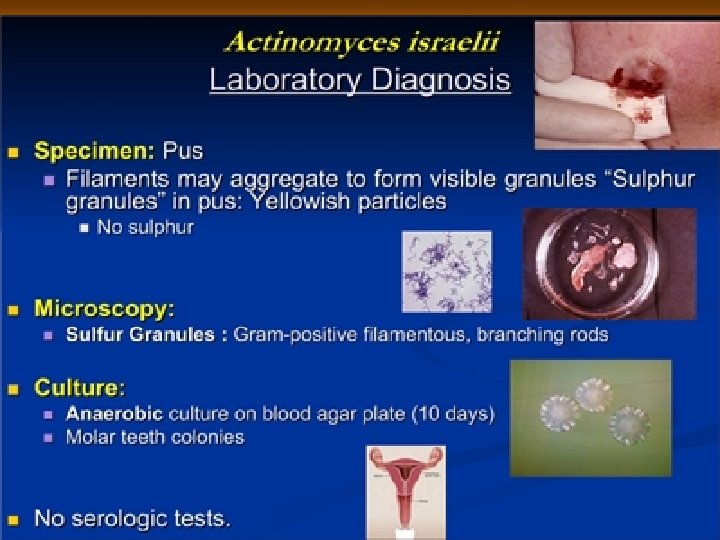
Actinomycosis ► Actinomyces israelii causes actinomycosis in which chronic granulomas become suppurative. ► Cervicofacial actinomycosis most common (~60%), followed by abdominal (20%) and pulmonary actinomycosis(15%). ► Tissue pus contains “sulfur granules”, a mass of branching bacteria. ► Presence of sulfur granules establishes a diagnosis of actinomycosis.

Anaerobic Actinomyces: Types of Infectious Disease-2 -
Aerobic Actinomycetes: Identification ► Rhodococcus, Gordonia, and Tsukamurella difficult to characterize biochemically. Identification is based on partial acid-fastness, colony morphology, and 16 S r. RNA gene sequence analysis ► Rhodococcus: slimy, salmon-pink colonies ► Gordonia: smooth, beige to salmon-pink colonies ► Tsukamurella: cerebroid, cream colonies
Anaerobic Actinomyces: Identification ► Actinomyces israelii is anaerobic with clinical strains varying from obligate anaerobes to microaerophilic ► A. israelii definitively is identified by detection using gas liquid chromatography (GLC) of acetic and lactic acid as end products of carbohydrate metabolism
Actinomycosis There at least five (5) types of actinomycosis ► Cervicofacial actinomycosis ► Thoracic actinomycosis ► Abdominal actinomycosis ► Pelvic actinomycosis ► Generalized actinomycosis
Actinomycosis ► Cervicofacial actinomycosis occurs in the mouth, neck and head region. ► The bacterium enters through the periodontium soft tissue wounds or salivary glands. ► Cervicofacial actinomycosis develops slowly. The area becomes hard, the overlying skin becomes reddish and swelling appears in the mouth and neck. ► Abscesses develop within and eventually drain to the surface where sulfur granules , masses of filamentous organisms, may be found in the pus.
Actinomycosis ► Thoracic actinomycosis involves the lungs and mediastinum ► The disease begins with fever, cough, and sputum production. The patient becomes weak, loses weight and may have night sweats and shortness of breath. ► Cervicofacial and thoracic disease may result in nervous system complications ; most commonly brain abscesses or meningitis.
Actinomycosis ► Abdominal actinomycosis are mostly preceded by surgery. ► Infection usually begins in the gastrointestinal tract and spreads to the abdominal wall. ► Fever and chills, intestinal colic, vomiting, and weight loss, a palpable (can be felt) mass and an external sinus are evident in this type of actinomycosis.
Actinomycosis ► Pelvic actinomycosis affects the women's pelvic area and may cause lower abdominal pain, fever, and bleeding between menstrual periods. This form of the infection has been associated with the use of IUDs (intra-uterine devices) that do not contain copper. ► Generalized actinomycosis may involve the skin, brain, liver and urogenital system.
Treatment ► Treatment for actinomycosis is long term, generally with up to one month of intravenous penicillin G, followed by weeks to months of penicillin taken by mouth. ► Additionally, surgical excision and drainage of abscesses may be necessary.

NOCARDIA SP
NOCARDIA SP ►Named after Edmond Nocard, ► In 1888 described the organism in cattle ► First human case of Nocardiosis was reported in 1890 by Eppinger.
NOCARDIA : Classification ► Gram-positive bacteria. ► On microscopy have branching filamentous cells. ► Members of the group are often only distantly related phylogenetically. ► Part of a subgroup of aerobic nocardiform actinomycetes includes: Mycobacterium, Corynebacterium, Nocardia, Rhodococcus, Gordona, and Tsukamurella and the cause of Whipple's disease (Tropheryma whippeli).
NOCARDIA : Classification ► Standard laboratory techniques are limited in their ability to differentiate these organisms. ► Molecular genetics have identified at least 30 species, 13 of which cause human infection. ► The more common human pathogen are Nocardia asteroides sensu stricto, Nocardia farcinica, Nocardia nova, Nocardia brasiliensis, Nocardia pseudobrasiliensis, Nocardia otitidiscaviarum, and Nocardia transvalensis.
NOCARDIA : Epidemiology ► Nocardia is everywhere in the environment: soil, organic matter, and water. ► Human infection usually occurs from minor trauma and direct inoculation of the skin or soft tissues or by inhalation. It is also a common animal infection ► Outbreaks in oncology and transplant wards and surgical wounds have occurred from fomites, hospital construction with resultant contaminated dust, and health care worker hands.
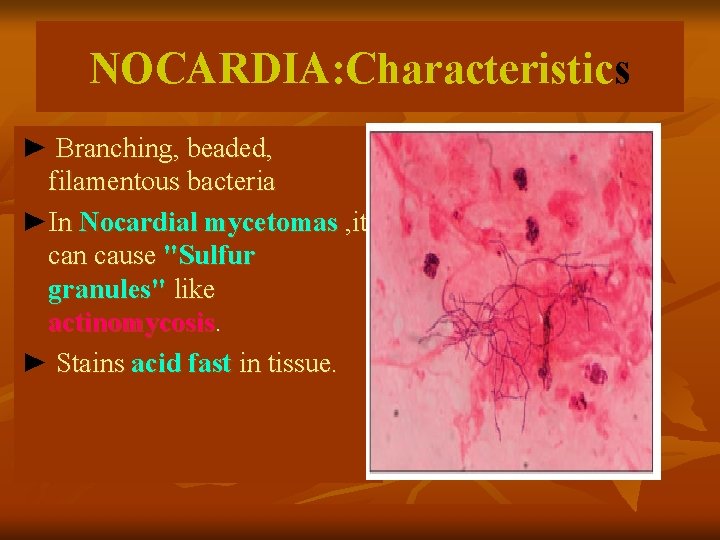
NOCARDIA: Characteristics ► Branching, beaded, filamentous bacteria ►In Nocardial mycetomas , it can cause "Sulfur granules" like actinomycosis. ► Stains acid fast in tissue.
NOCARDIA: Virulence ► Virulent strains are relatively resistant to neutrophilmediated killing. ► Organisms in the logarithmic growth phase are more toxic to macrophages. ► Inhibit phagosome-lysosome fusion more successfully in vitro, which gives rise to L-forms, which can survive in macrophages for days ► L-forms have been found in human and animal infections and perhaps account for treatment failure.
NOCARDIA: Virulence There are species tissue tropism's: ► N. asteroides complex including N. farcinica cause 80% of noncutaneous invasive disease and most systemic and CNS (Central Nervous System) disease. ► N. brasiliensis: Cutaneous and lymphocutaneous disease. ► N. pseudobrasiliensis: Systemic infections, including the CNS. ► N. transvalensis and N. otitidiscavarium: Noncutaneous disease
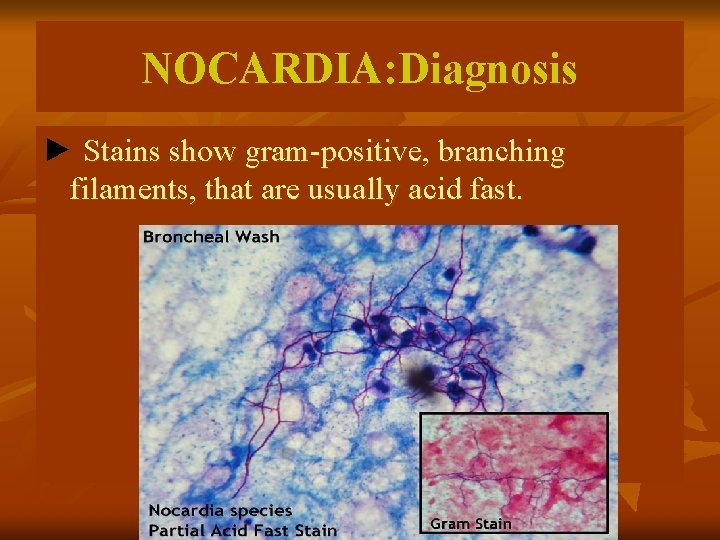
NOCARDIA: Diagnosis ► Stains show gram-positive, branching filaments, that are usually acid fast.
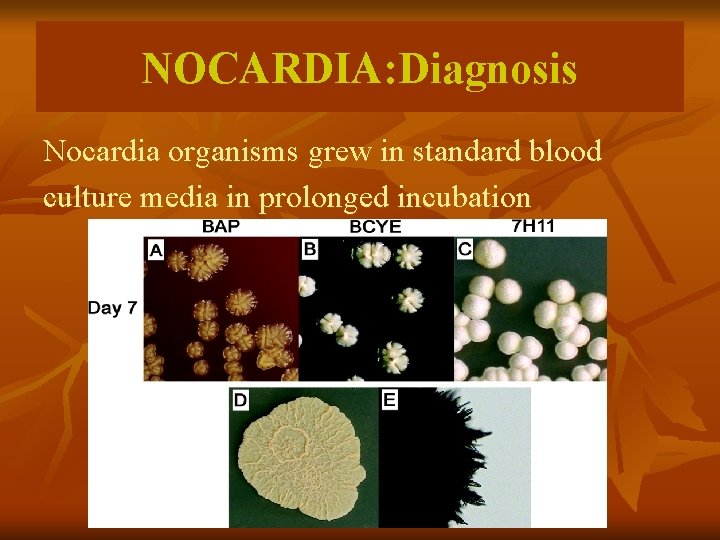
NOCARDIA: Diagnosis Nocardia organisms grew in standard blood culture media in prolonged incubation
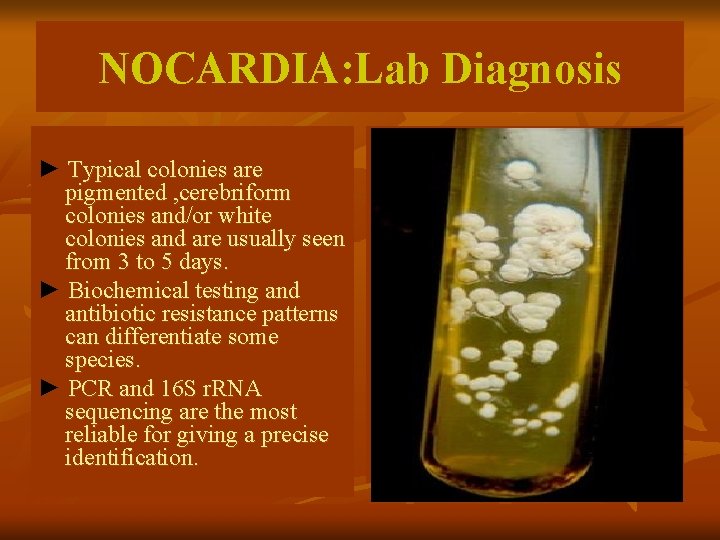
NOCARDIA: Lab Diagnosis ► Typical colonies are pigmented , cerebriform colonies and/or white colonies and are usually seen from 3 to 5 days. ► Biochemical testing and antibiotic resistance patterns can differentiate some species. ► PCR and 16 S r. RNA sequencing are the most reliable for giving a precise identification.

Nocardia on blood agar
Risk Factors for Nocardiosis ► Immunocompromise host: 60% of all reported nocardiosis is associated with preexisting immune dysfunction. ►Organ transplantation, hematologic malignancy, alcoholism, steroid use, diabetes, acquired immunodeficiency syndrome (AIDS). and Patients with chronic pulmonary disorders are in risk.
Clinical Syndromes: Mucocutaneous ► Can occur after minor trauma and animal or insect bites; may also colonize open wounds. ► N. brasiliensis commonly causes a progressive cutaneous and lymphocutaneous (sporotrichoid) disease. ► N. asteroides more commonly causes self-limited infection.
Clinical Syndromes: Mucocutaneous ► Mycetoma: a chronic progressive, destructive disease, occurring days to months after inoculation ► Located distally on the limbs (classically the foot) and is present with n n n Suppurative granulomata Progressive fibrosis and necrosis Sinus formation and destruction of adjacent structures, Macroscopically visible infective granules Mimics fungal mycetoma and actinomycetomata

Mucocutaneous Nocardiosis
Clinical Syndromes: Pulmonary ●Pulmonary disease is the most common reported. ● Bacteria colonize sputum of COPD patients. ● Clinical Presentations: ► endobronchial inflammatory masses pneumonia ► lung abscess, ► cavitary disease ► empyema ► pneumonia (often progressive in HIV) ► it can invade through surrounding tissues like actinomycosis
Clinical Syndromes ► Cardiac Conditions Nocardia has been highly linked to endocarditis as a main symptom. In recorded cases, it has caused damage to heart valves. ► Ocular disease Very rarely Nocardia cause keratitis, generally after trauma
Disseminated Nocardiosis ► Disseminated infection can occur in very immunocompromised patients, through the spreading enzymes possessed by the bacteria. ►It generally involves both lungs and brain ► Multiple cavitating pulmonary infiltrates develop ► Cerebral abscesses arise later ► If untreated, the prognosis is poor for this form of disease
Treatment ► Nocardiosis requires at least 6 months of treatment, preferably with co-trimoxazole or high doses of sulfonamides. ► In patients who don’t respond to sulfonamide treatment, other drugs, such as ampicillin, erythromycin, or minocycline may be added. ► Treatment also includes surgical drainage of abscesses and excision of necrotic tissue. ► A new combination drug therapy (sulfonamide, ceftriaxone and amikacin) is also in usage.
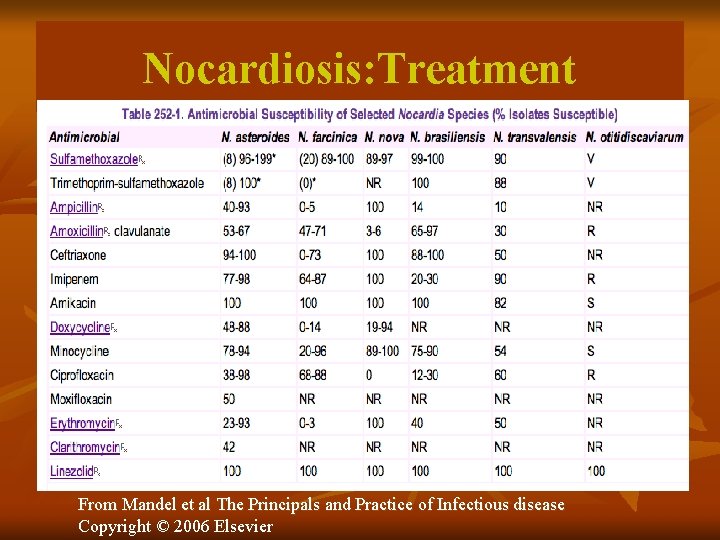
Nocardiosis: Treatment From Mandel et al The Principals and Practice of Infectious disease Copyright © 2006 Elsevier
- Slides: 44
Từ khóa » Hrisi Bahar
-
Prof.Dr. Hrisi BAHAR TOKMAN | AVESİS
-
Hrisi BAHAR | Professor (Full), PhD In Clinical Microbiology.
-
Hrisi Bahar Tokman (0000-0002-2205-5120) - ORCID
-
Hrisi Bahar | Facebook
-
Hrisi BAHAR TOKMAN - Öğretim Üyesi - LinkedIn
-
Doç. Dr. Hrisi Bahar: “Bilimle Uğraşmak Bir çeşit Yaşama Bi&
-
Hrisi Bahar Profesör Oldu | Şalom Gazetesi - 27.07.2022
-
Uzm. Dr. Hrisi Bahar - Yorumları Incele Ve Randevu Al
-
Hrisi Bahar Tokman - Wikidata
-
HRİSİ BAHAR TOKMAN | TR Dizin
-
Hrisi Bahar-Tokman