Prediction Of Massive Bleeding. Shock Index And Modified Shock Index
Có thể bạn quan tâm
- Home
- All contents
- Ahead of print
- Latest issue
- All issues
- Special issues & Supl.
- Covers gallery
- Subscribe to our newsletter
- Publish your article
- Guide for authors
- Submit an article
- Ethics in publishing
- Open Access Option
- Language Editing services
- Visual abstract
- About the journal
- Aims and scope
- Editorial Board
- Subscribe
- Junta directiva SEMICYUC
- Junta directiva FEPIMCTI
- Advertising
- Metrics
- Most often read last 3 years
- All metrics
- Metrics by country
 ISSN: 2173-5727
ISSN: 2173-5727 Medicina Intensiva is the journal of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (SEMICYUC), and has become the reference publication in Spanish in its field. Medicina Intensiva mainly publishes Original Articles, Reviews, Clinical Notes, Images in Intensive Medicine, and Information relevant to the specialty. All works go through a rigorous selection process.
See moreSend a Visual Abstract to expand the reach of your research.
Indexed in:Medline
See more Follow us: Twitter RSS Alerta email Subscribe: Impact factor
Impact factor The Impact Factor measures the average number of citations received in a particular year by papers published in the journal during the two preceding years. © Clarivate Analytics, Journal Citation Reports 2025
See more Impact factor 2024 3.1 CitescoreCiteScore measures average citations received per document published.
See more Citescore 2024 2.3 SJRSRJ is a prestige metric based on the idea that not all citations are the same. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal's impact.
See more SJR 2024 0.353 SNIPSNIP measures contextual citation impact by wighting citations based on the total number of citations in a subject field.
See more SNIP 2024 0.573 View more metrics Open Access option Hide Journal Information Previous article | Next article Vol. 41. Issue 9.Pages 532-538 (December 2017) Lee este artículo en Español Export reference Share Share Twitter Facebook Bluesky Linkedin whatsapp E-mail Print Download PDF More article options Statistics Outline- Abstract
- Keywords
- Resumen
- Palabras clave
- Introduction
- Abstract
- Keywords
- Resumen
- Palabras clave
- Introduction
- Design and methods
- Results
- Discussion
- Conclusions
- Authorship
- Conflicts of interest
- Acknowledgements
- Bibliography
 Tables (2) Table 1. Diagnostic determination of the shock index and modified shock index.
Tables (2) Table 1. Diagnostic determination of the shock index and modified shock index. 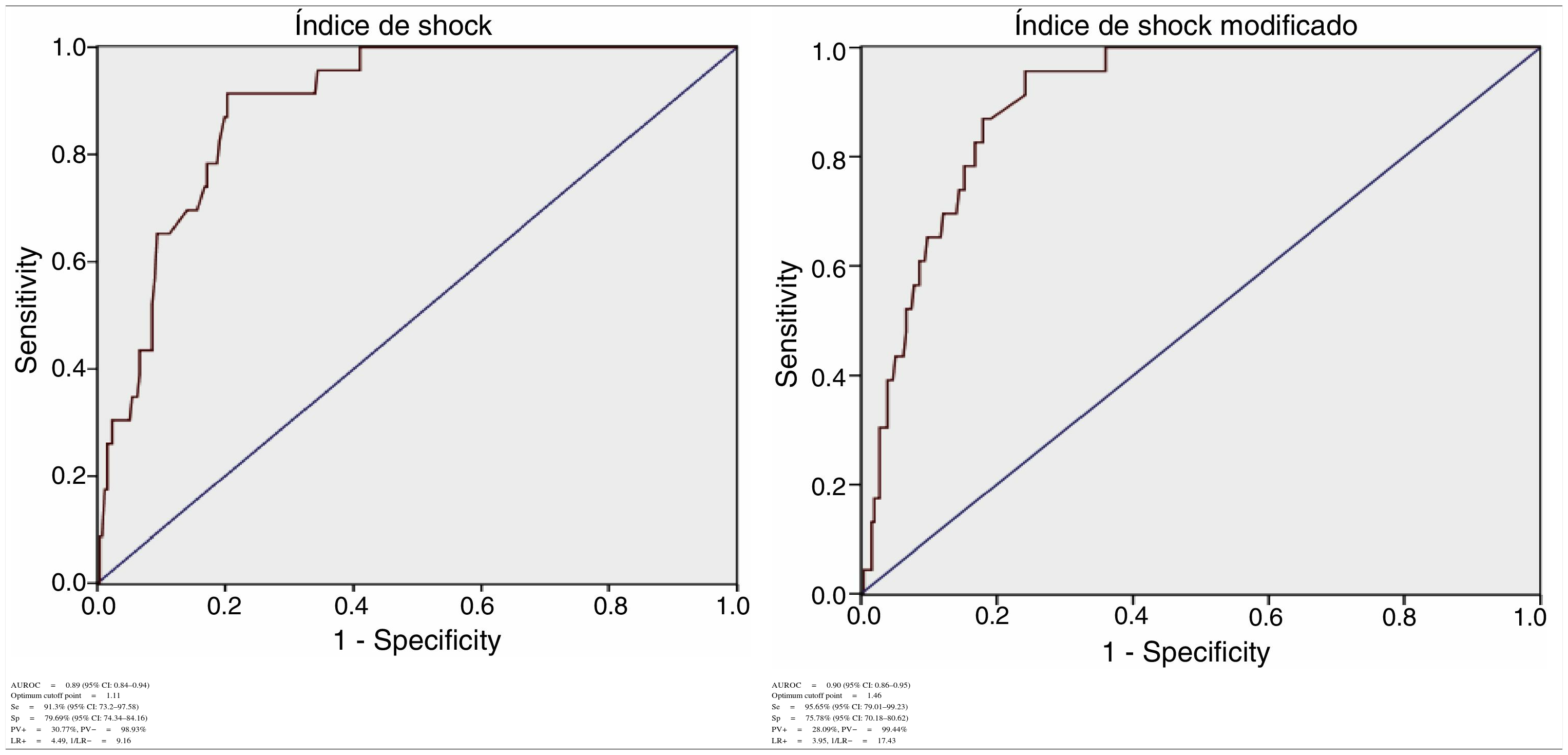 Table 2. Characteristics of the patients according to the shock index and modified shock index.
Table 2. Characteristics of the patients according to the shock index and modified shock index. 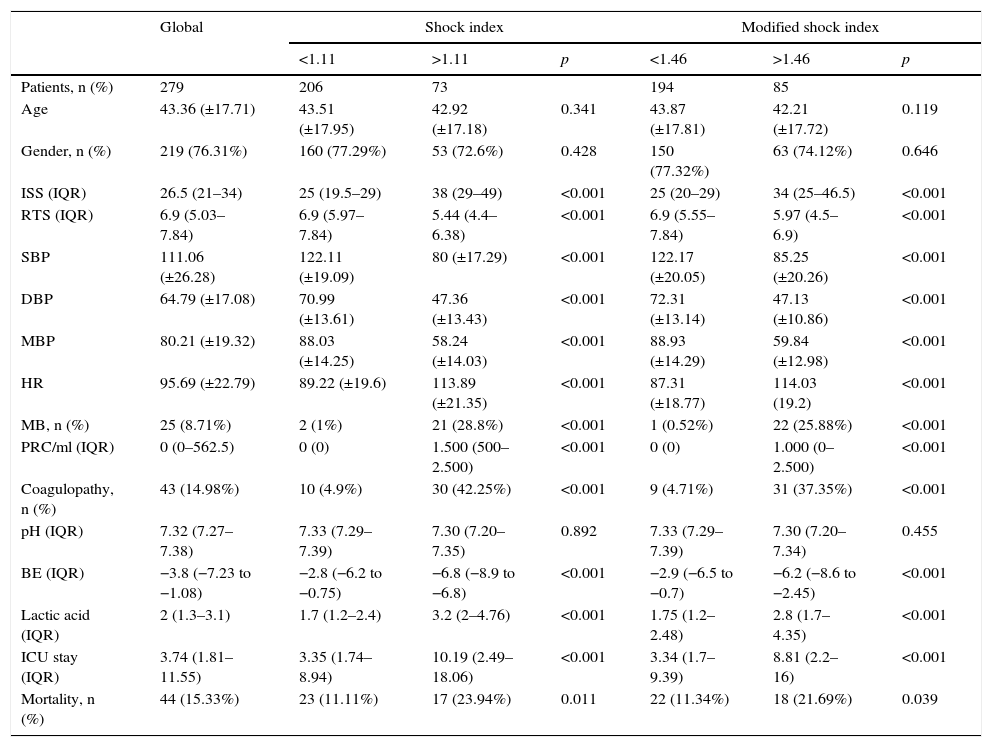 AbstractObjective
AbstractObjectiveTo determine the predictive value of the shock index and modified shock index in patients with massive bleeding due to severe trauma.
DesignRetrospective cohort.
SettingSevere trauma patient's initial attention at the intensive care unit of a tertiary hospital.
SubjectsPatients older than 14 years that were admitted to the hospital with severe trauma (injury severity score >15) form January 2014 to December 2015.
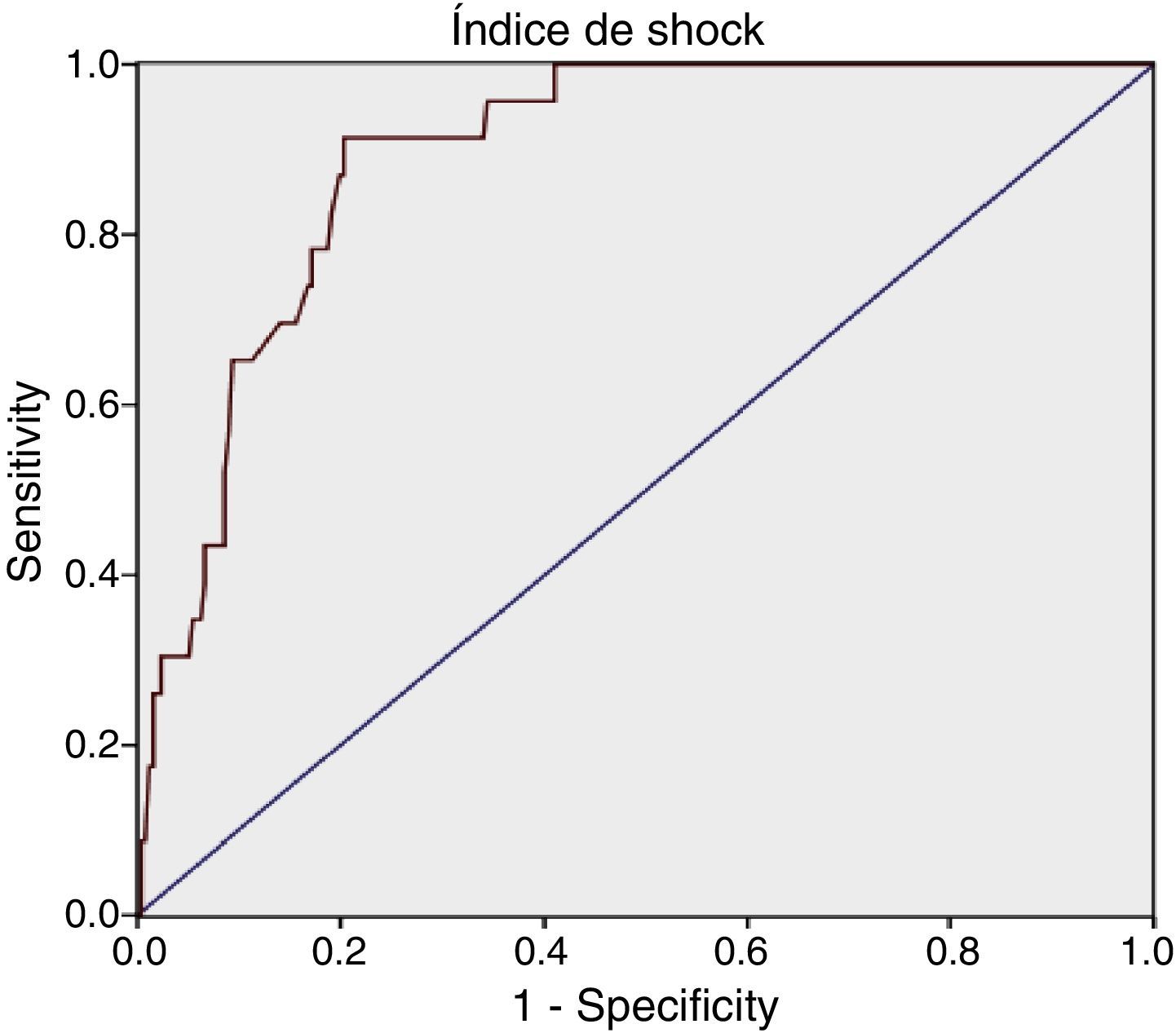
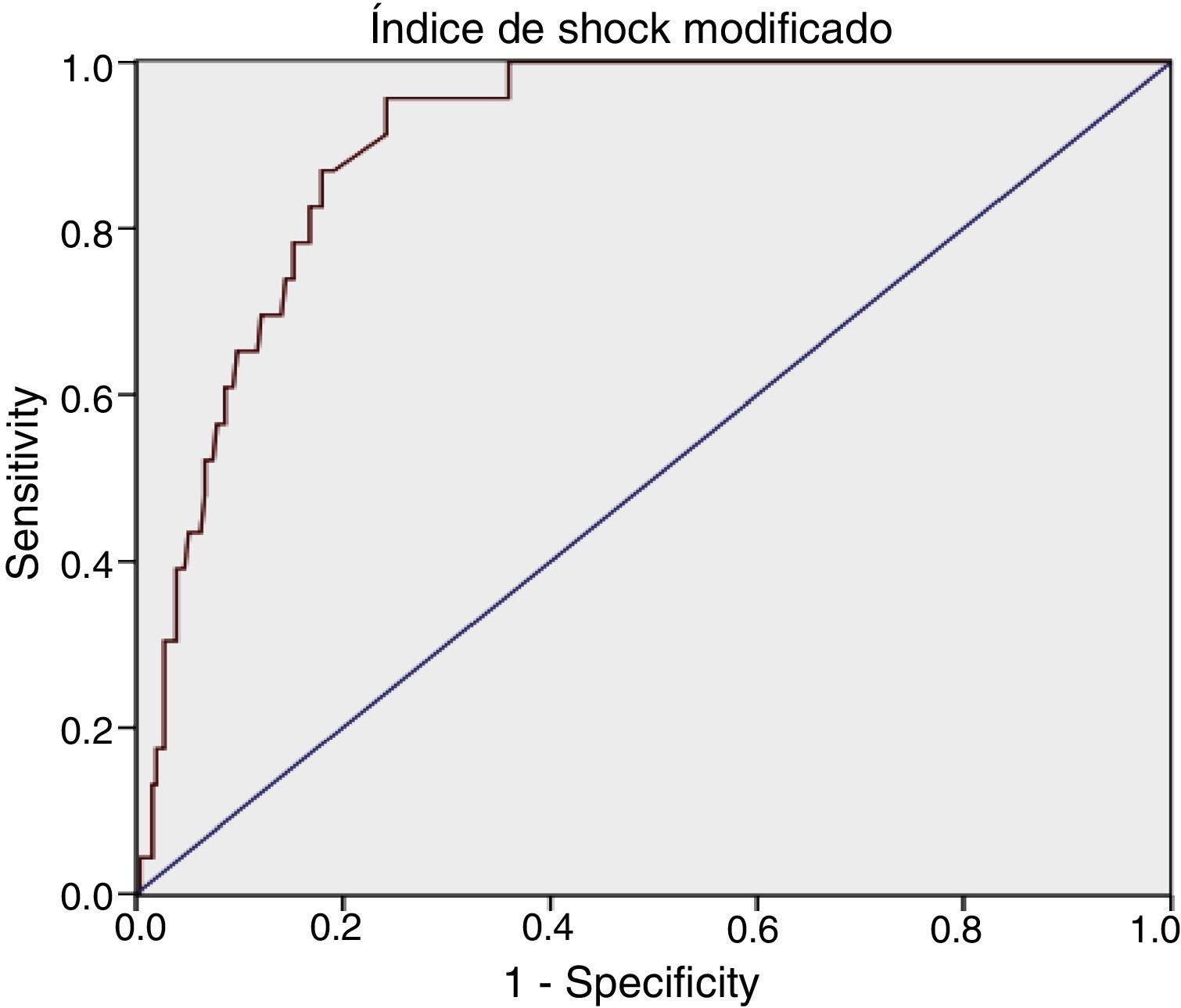
VariablesWe studied the sensitivity (Se), specificity (Sp), positive and negative predictive value (PV+ and PV−), positive and negative likelihood ratio (LR+ and LR−), ROC curves (receiver operating characteristics) and the area under the same (AUROC) for prediction of massive hemorrhage.
Results287 patients were included, 76.31% (219) were male, mean age was 43.36 (±17.71) years and ISS was 26 (interquartile range [IQR]: 21–34). The overall frequency of massive bleeding was 8.71% (25). For shock index: AUROC was 0.89 (95% confidence intervals [CI] 0.84–0.94), with an optimal cutoff at 1.11, Se was 91.3% (95% CI: 73.2–97.58) and Sp was 79.69% (95% CI: 74.34–84.16). For the modified shock index: AUROC was 0.90 (95% CI: 0.86–0.95), with an optimal cutoff at 1.46, Se was 95.65% (95% CI: 79.01–99.23) and Sp was 75.78% (95% CI: 70.18–80.62).
ConclusionShock index and modified shock index are good predictors of massive bleeding and could be easily incorporated to the initial workup of patients with severe trauma.
Keywords:Massive bleedingMassive transfusionShock indexModified shock indexInjury severity scoreRevised trauma scoreResumenObjetivoDeterminar la capacidad de predicción del índice de shock y del índice de shock modificado para hemorragia masiva tras sufrir un trauma grave.
DiseñoCohorte retrospectiva.
ÁmbitoAtención inicial hospitalaria al paciente con enfermedad traumática grave en una unidad de cuidados intensivos de trauma de un hospital terciario.
SujetosPacientes mayores de 14 años con trauma grave (injury severity score [ISS]>15), admitidos de forma consecutiva desde enero de 2014 hasta diciembre de 2015.
VariablesSe estudiaron sensibilidad (Se), especificidad (Sp), valores predictivos positivo y negativo (VP+ y VP−), razones de verosimilitud positiva y negativa (RV+ y RV−), curvas ROC (receiver operating characteristics) y el área bajo las mismas (AUROC) para predicción de hemorragia masiva.
ResultadosSe incluyeron 287 pacientes, el 76,31% (219) fueron varones, con una edad media de 43,36 (±17,71) e ISS de 26 (rango intercuartil [RIC]: 21-34). La frecuencia global de hemorragia masiva fue de 8,71% (25). Para el índice de shock se obtuvo: AUROC de 0,89 (intervalo de confianza [IC] 95%: 0,84-0,94), con un punto de corte óptimo en 1,11, Se del 91,3% (IC 95%: 73,2-97,58) y Sp del 79,69% (IC 95%: 74,34-84,16). Para el índice de shock modificado se obtuvo: AUROC de 0,90 (IC 95%: 0,86-0,95), con un punto de corte óptimo en 1,46, Se del 95,65% (IC 95%: 79,01-99,23) y Sp del 75,78% (IC 95%: 70,18-80,62).
ConclusionesEl índice de shock y el índice de shock modificado son buenos predictores de hemorragia masiva y de fácil aplicación durante la atención inicial del trauma grave.
Palabras clave:Hemorragia masivaTransfusión masivaÍndice de shockÍndice de shock modificadoEscala de severidad del traumaEscala de trauma revisado Full Text IntroductionHemorrhagic shock is the leading cause of avoidable mortality following severe trauma. Its early identification remains a challenge both out and in hospital–a fact that results in deficient diagnosis and inappropriate patient transfer.1,2
The early diagnosis of hemorrhagic shock is essential to improve the outcomes after trauma and control bleeding. Early and precise prediction of hemorrhagic shock makes it possible to adequately prepare the initial patient management team, with prompt activation of the massive bleeding protocol (MBP).3–5
Retrospective studies analyze different predictive indices, assessing their capacity to diagnose massive bleeding (MB). These indices are difficult to implement, however: their determination requires laboratory test results and imaging data that are very time consuming and difficult to perform at out-hospital level.6
On the other hand, simple clinical parameters such as heart rate or arterial pressure have been shown to be inexact in predicting MB.7–9
The shock index (SI), defined as heart rate divided by systolic blood pressure, and the modified shock index (MSI), defined as heart rate divided by mean blood pressure, are simple and easy to apply, and have therefore been studied by a number of authors.
Different studies have shown that a high SI after severe trauma is associated to high mortality10–12 and to the severity of injury.13 The SI has also been used as a predictor of days on mechanical ventilation and of hospital stay,14 as well as of the probability of admission to critical care.15 Lastly, some authors have related SI to the need for blood transfusion and hemostatic intervention.16 Less is known of its capacity to predict MB, however.
The present study was carried out to determine the capacity of SI and MSI to define the optimum cutoff point in patients who have suffered severe trauma.
Design and methodsA retrospective cohort study involving the consecutive inclusion of all patients was carried out in the trauma and emergencies intensive care unit (ICU) of a tertiary hospital. We included patients over 14 years of age with severe trauma (injury severity score [ISS] >15) in which initial management took place upon arrival in hospital. The study patients were admitted between January 2014 and December 2015 (excluding individuals with cardiorespiratory arrest in out-hospital care, spinal cord injury, the use of heart rate-regulating drugs, and initial resuscitation performed in another center). Initial trauma care is provided by a specialized team composed of two intensivists (staff physician and resident), two nurses, a clinical assistant and two hospital attendants. The team can also consult different specialists related to trauma care. Management is carried out following the Advanced Trauma Life Support (ATLS) guidelines. The hospital has a MBP that has been approved by the transfusions commission and by hospital management.
The data were collected with masking of the observer: demographic variables (age and gender), physiological parameters (first recorded heart rate, systolic and diastolic blood pressure after arrival in hospital–initial resuscitation area of the ICU); laboratory test parameters (arterial blood gases–pH, base excess [BE], lactic acid) and prognostic variables (revised trauma score [RTS], ISS). The transfusions registry of our unit was consulted to document the number of packed red cell units transfused in the first 24h in each patient. Massive bleeding was defined as the administration of 10 or more packed red cell units in the first 24h of admission after trauma. Mathematical calculation of SI and MSI was subsequently made. As commented above, SI was defined as heart rate divided by systolic blood pressure, and MSI was defined as heart rate divided by mean blood pressure. No determination of MSI was made in patients without diastolic blood pressure. Lastly, we consulted the discharge reports to assess hospital stay and mortality.
Qualitative variables were reported as frequency and proportion, while quantitative variables were reported as the mean (±standard deviation) and median (interquartile range [IQR]). The χ2 test and Fisher exact test were used to estimate the association between two categorical variables, while the Student t-test was used for the comparison of two means (after checking normal distribution of the data with the Kolmogorov–Smirnov test, and homogeneity of variances with the Levene test). The Wilcoxon test was used in the case of a non-normal distribution. Statistical significance was considered for p≤0.05.
For each index we calculated sensitivity, specificity, positive predictive value (PV+), negative predictive value (PV−), positive likelihood ratio (LR+) and negative likelihood ratio (LR−). The receiver operating characteristic (ROC) curves were obtained, with calculation of the area under the curve (AUROC) and the corresponding 95% confidence interval (95% CI). The SPSS® version 19.0 statistical package for MS Windows was used throughout.
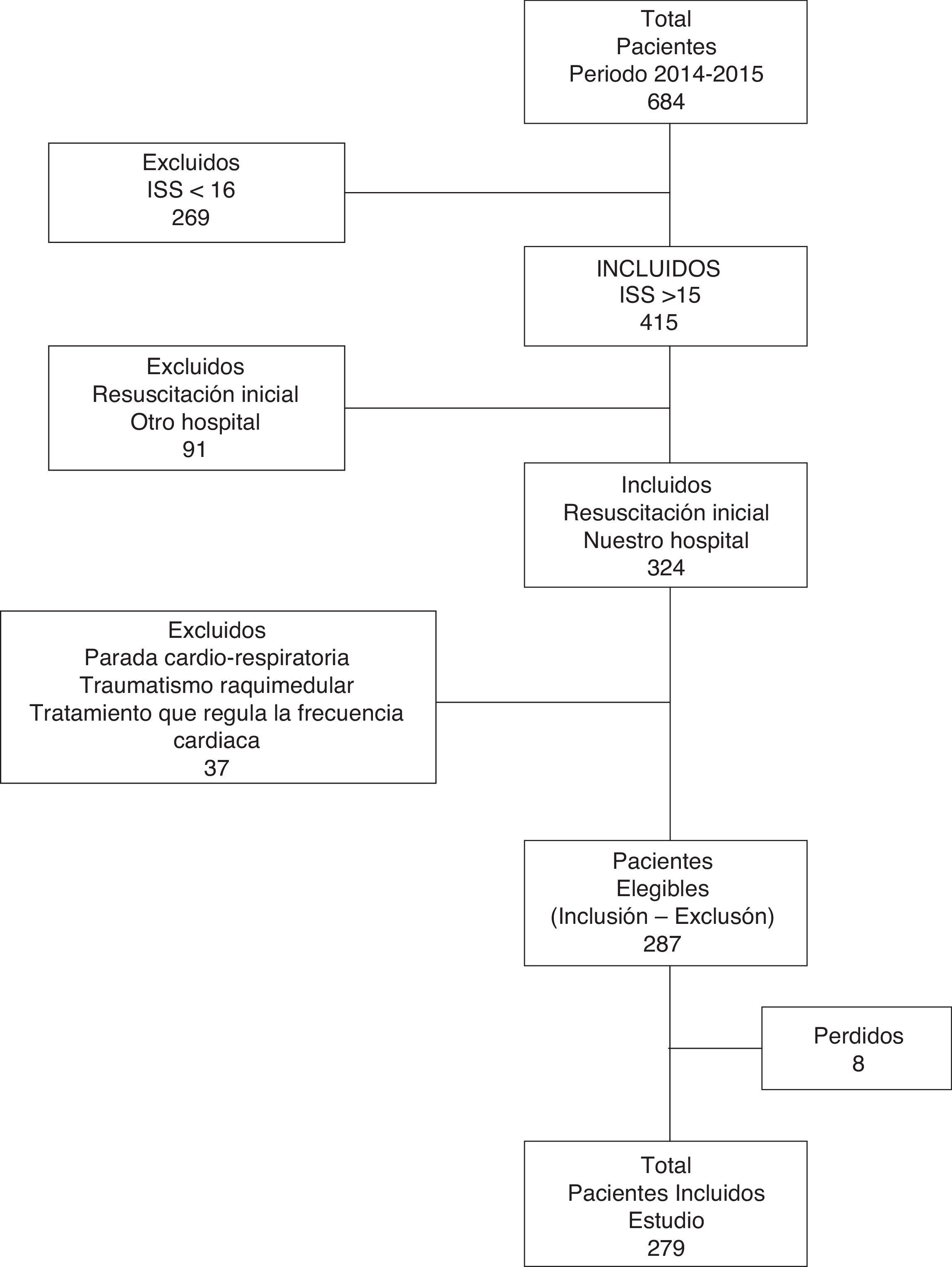
ResultsA total of 287 patients were studied (Fig. 1). Of these, 76.31% (n=219) were men. The mean age was 43.36 (±17.71) years and the median ISS score was 26 (IQR: 21–34). Closed trauma represented 91.6% of the cases (falls from a height being the most frequent cause). The overall MB rate was 8.71% (n=25); the median duration of stay in the ICU was 3.74 days (IQR: 1.81–11.55); and the mortality rate was 15.33% (n=44).
 Figure 1.
Figure 1. Flow of patients included in the study. Period 2014–1015.
For SI we obtained: AUROC 0.89 (95% CI: 0.84–0.94), with an optimum cutoff point of 1.11, sensitivity 91.3% (95% CI: 73.2–97.58) and specificity 79.69% (95% CI: 74.34–84.16).
For MSI we obtained: AUROC 0.90 (95% CI: 0.86–0.95), with an optimum cutoff point of 1.46, sensitivity 95.65% (95% CI: 79.01–99.23) and specificity 75.78% (95% CI: 70.18–80.62) (Table 1).
Table 1.Diagnostic determination of the shock index and modified shock index.
 |  |
| AUROC=0.89 (95% CI: 0.84–0.94)Optimum cutoff point=1.11 | AUROC=0.90 (95% CI: 0.86–0.95)Optimum cutoff point=1.46 |
| Se=91.3% (95% CI: 73.2–97.58) | Se=95.65% (95% CI: 79.01–99.23) |
| Sp=79.69% (95% CI: 74.34–84.16) | Sp=75.78% (95% CI: 70.18–80.62) |
| PV+=30.77%, PV−=98.93% | PV+=28.09%, PV−=99.44% |
| LR+=4.49, 1/LR−=9.16 | LR+=3.95, 1/LR−=17.43 |
AUROC: area under the ROC curve; CI: confidence interval; LR+: positive likelihood ratio; LR−: negative likelihood ratio; Se: sensitivity; Sp: specificity; PV+: positive predictive value; PV−: negative predictive value.
An a posteriori analysis was made with the defined cutoff points, contrasting different variables to obtain significant differences for MB, the severity of injury (ISS), coagulopathy, ICU stay and mortality (Table 2).
Table 2.Characteristics of the patients according to the shock index and modified shock index.